Heart failure (cardiac insufficiency)
Heart failure means the inability of the heart muscle to pump enough oxygen-enriched blood into the circulation, which can lead to an insufficient supply of blood or oxygen and nutrients to all organs/body cells. This results in typical symptoms such as reduced physical performance, shortness of breath and water retention (see below).
The risk of developing heart failure over the course of a lifetime is around 20%. 1-2% of the adult population suffer from heart failure, whereby it mainly affects people of advanced age, as the rate of new cases roughly doubles per decade of life.
However, the significantly improved treatment options for heart failure over the last 10 years have led to a considerable improvement in the prognosis and symptoms of the disease.
Overall, the occurrence of heart failure can also be positively influenced by influencing lifestyle and risk factors in older people, which is why efforts to control cardiovascular risk factors (smoking, high blood pressure, high cholesterol, obesity) should be intensively supported.
Causes
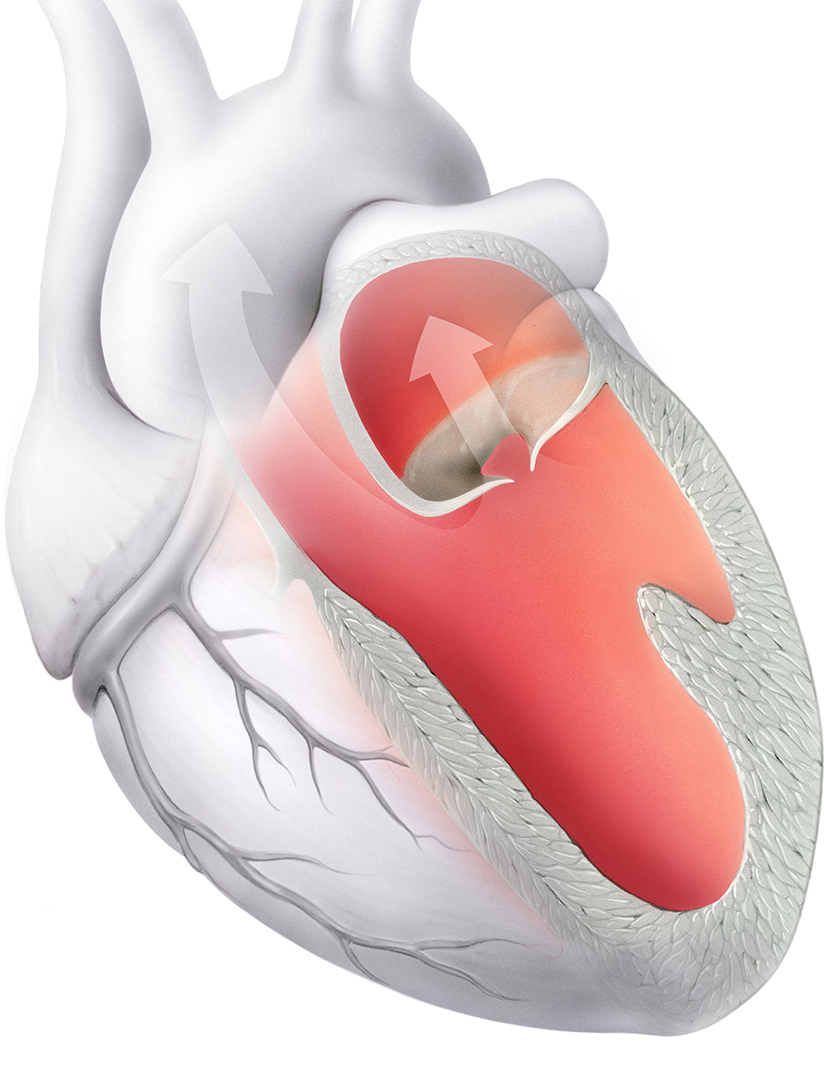
Heart failure can be the final stage of various disease processes in the heart muscle, such as structural or functional changes, e.g. thickening of the heart muscle, enlargement of the heart muscle with reduced pumping function (congenital or, for example, after a heart attack or myocarditis), heart valve defects or cardiac arrhythmia (Fig. 1). Heart failure can also be caused by age-related or congenital heart valve diseases.
Heart failure does not occur as a stand-alone disease, but usually as a result of an underlying cardiac condition, especially in older patients who are often already undergoing medical treatment for other illnesses. Consequently, the majority of patients have concomitant diseases, e.g. angina pectoris, high blood pressure, diabetes mellitus, lung diseases.
Common problems in heart failure patients can have many causes (e.g. renal insufficiency), while others cannot be explained in detail (anemia, hypotension, cachexia, respiratory disorders). The existence of multiple comorbidities represents a potential for drug intolerance and drug interactions and makes the management of patients with heart failure particularly complex.
Symptoms
Symptomatic signs of heart failure include signs of reduced peripheral blood flow with contraction of the small vessels, as well as signs of water retention in the lungs, abdomen and legs. Typical signs are
- Reduced performance with shortness of breath, fatigue during physical exertion
- Difficulty breathing when lying flat in bed
- Shortness of breath during the smallest activities such as tying shoes
- Decreased appetite with a feeling of pressure in the right upper abdomen, constipation
- Swelling of the legs/lower legs
- Dizziness/fainting
- Low BD values
Furthermore, cardiac insufficiency can lead to cardiac arrhythmias from the main (ventricular tachycardia with the risk of sudden cardiac death) and the atria (such as atrial fibrillation).
Heart failure with normal versus impaired cardiac output
While heart failure with impaired heart pumping function (systolic dysfunction) is based on an impairment of muscle contraction, heart failure with normal pumping function but "stiffened" small heart muscle is the result of impaired "relaxation" with reduced filling of the ventricles (but preserved ejection function).
Acute heart failure
Acute heart failure is a suddenly occurring, rapidly worsening condition. It can be caused by an acute deterioration in the heart's pumping capacity in the presence of pre-existing heart disease (e.g. chronic heart failure, heart valve disease, etc.), or by an acute cardiac event with previously normal myocardial function (e.g. acute myocardial infarction or acute myocarditis). Specially trained cardiology teams can usually achieve a rapid improvement with acute, specific therapy. The extreme form of acute heart failure is cardiogenic shock, with a high mortality rate due to the risk of multiple organ failure.
Diagnosis of heart failure
Many of the main symptoms such as shortness of breath, fatigue and leg swelling are not specific and are sometimes particularly difficult to interpret (especially in older patients), leading to a number of differential diagnostic considerations. The symptoms may also be a side effect of certain medications. It is therefore of the utmost importance that a correct diagnosis is made and the best possible treatment for the patient is initiated by a specialized team.
Diagnostics
- Medical history and physical examination by a cardiologist
- Resting ECG
- Certain blood tests
- Cardiac ultrasound examination or cardiac MRI to assess cardiac performance and valves, indications of myocarditis that has taken place
- In the event of an acute or previous myocardial infarction or coronary artery stenosis, a cardiac catheter examination with widening of the stenosed vessels/stent implantation, evaluation of a bypass operation in the case of multiple coronary artery stenoses if necessary
These help to determine the causes and severity of the disease on the one hand, and on the other hand represent a guide for further therapy, e.g. an indication for surgical/catheter-based therapy for valve diseases, an indication for special pacemakers or defibrillators (see below), as well as the initiation of specific drug therapy, depending on the cause of the cardiac output and other factors, e.g. renal insufficiency, chronic lung disease or diabetes mellitus.
Therapy options
- Cardiac catheterization and treatment of coronary artery stenosis, bypass surgery if necessary
- Heart valve operations (surgical or catheter-based)
- Drug therapy:
- The foundation of heart failure therapy lies in modern drug treatment. In this area in particular, substantial progress has been made over the past 5 years, with significant improvements in both symptoms and survival. The aim of the medication is to relieve the heart, dilate the blood vessels, achieve optimum blood ejection, adjust blood pressure and optimally adapt water tablets. Furthermore, the heart medication reduces stress on the heart muscle and counteracts cardiac arrhythmia. However, the therapy must be initiated and adapted individually for each patient.
- Depending on the cardiac output/underlying disease, common/typical heart failure medications used are:
- Inhibitors of the renin-angiotensin-aldosterone system (ACE inhibitors, sartans, sacubitril-valsartan, aldosterone antagonists)
- Beta blockers
- Water tablets
- Medication for cardiac arrhythmia (Amiodarone, Digoxin)
- SGLT-2 inhibitors
- Optimization of risk factors: dietary optimization, smoking cessation, physical activity, blood pressure and diabetes control, treatment of iron deficiency... all these factors are re-evaluated at each doctor's visit
- Special pacemakers/defibrillators: (see below)
- Cardiac resynchronization therapy (CRT):
- Implantation of a defibrillator
Our integrative therapy concept for heart failure
However, comprehensive advice/explanation of the patient's condition and therapeutic measures by the treating cardiologist is and remains of the utmost importance. What measures should be taken in everyday life, what needs to be done if etc.?
Repeated checks to assess the course of the disease/therapy success are necessary in order to make adjustments if necessary
Highly trained specialists in the team, e.g. for the treatment/sclerotherapy of cardiac arrhythmias, implantation of special pacemakers, performance of complex cardiovascular and heart valve interventions and operations, specialists for the treatment of advanced cardiac insufficiency and evaluation of heart transplantation/heart replacement procedures
A family history is also taken in order to identify any indications of hereditary heart disease and then a genetic screening examination can be carried out, as well as cardiac ultrasound examinations of relatives.




Interventional Cardiology